Services
Services We Provide

Orofacial Myofunctional Treatment
Orofacial myofunctional treatment is essentially physical therapy for the mouth, face, and airway. Exercises are strategically prescribed to strengthen the lip, tongue, and facial muscles, and restore functional breathing to help improve chewing, swallowing, speech, posture, and systemic functions.
Treatment aims to build awareness, strength, and coordination of the oral and facial muscles in order to meet these primary objectives:
- Getting the tongue resting in its proper position,
- Keeping the lips closed when the mouth is not in use,
- Optimizing healthy chewing, and
- Utilizing a proper initial-phase swallowing pattern.
In working towards these goals, treatment contributes to optimal growth, development, and function of the head, jaw, and airway. Subsequently, symptoms related to jaw/TMJ problems, sleep disordered breathing, digestive concerns, etc. may be alleviated when these tasks are accomplished habitually.
The ultimate treatment focus is on the airway because, above all, we need to breathe efficiently and effectively in order to survive and thrive. Some of the factors that affect the airway, and that are subsequently considered in my assessment and treatment approach, include:
- Tongue appearance, positioning, & function
- Tonsil & adenoid health
- Habitual mouth breathing vs. nasal breathing
- Tongue and lip-ties, as well as pre- & post-release rehabilitation
- Orthodontic treatments
- Diet/nutrition and digestion
- Chewing and swallowing techniques
- Speech and articulation
- Structure, function, & symptoms of the jaw, neck, & face
- Posture and biomechanics
- Breathing mechanics
- Fascial restrictions
- Oral habits
- Sleep quantity and quality
- Sleep disordered breathing
- General health
- And more…
Nasal Breathing Re-Education
“How often should you breathe through your mouth? As often as you eat through your nose!” Though I can’t recall who said it, the first time I heard this, it made me chuckle. Then it made me think. While it sounded like a silly thing to say, it was also a bit sobering.
I would guess that you’ve never eaten through your nose, but have you ever breathed through your mouth? I know I have. The caveat here is that while it is actually okay to breathe through your mouth on occasion, as when lifting a heavy load, exercising intensely, or even temporarily when your nose is congested, breathing through the mouth more than 30% of the time is unhealthy.

- Allergies
- Asthma
- Enlarged tonsils and/or adenoids
- Chronic rhinitis or nasal congestion
- Deviated septum
- Nasal polyps
- Respiratory infections
- Stress
- Food sensitivities
- Diets heavy in inflammatory foods
- Tongue positioning low in the mouth
- Mirror neuron/learned behavior
- Habit
In order to change the habit of mouth breathing, the cause(s) need to be identified and addressed. Additionally, it must be recognized that a body accustomed to mouth breathing simply doesn’t know on its own how to nasal breathe normally for a couple of reasons – 1) Muscles of the mouth, face, and body have compensated and learned incorrect movement patterns over time, and 2) A mouth-breathing body has become used to suboptimal levels of carbon dioxide and oxygen within its system.
Orofacial myofunctional treatment helps to retrain the mouth and facial muscles, which is necessary for effectively managing mouth breathing by way of improving lip closure and minimizing compensations. In conjunction with this exercise-based approach, nasal breathing re-education further aims to gently restore functional nasal breathing, improve respiratory muscle function, and optimize oxygen uptake by essentially recalibrating the body’s respiratory physiology. Subsequently, when patients are effectively retrained to nasal breathe, dramatic changes to their overall health and quality of life can occur.
- Stimulates nasal nitric oxide production (helps fight infection, improve blood flow, increase lung volume)
- Optimizes oxygen absorption
- Maintains body temperature
- Improves brain function
- Reduces hypertension and stress
- Improves sleep quality
How Does Mouth Breathing Affect The Body?
Mouth breathing, or an open-mouth posture, leads to a number of detrimental effects on the mouth and body:
Just as a tongue that is positioned in the bottom of the mouth contributes to mouth breathing, mouth breathing likewise changes where the tongue rests in the mouth and how it functions.
Your tongue should naturally rest fully in the top of your mouth. However, when your mouth is open, the tongue is more likely to rest in the bottom. This leads to underdeveloped oral musculature and can contribute to abnormal mechanics during breathing, speech, chewing, and swallowing. Additionally, when the tongue rests low in the mouth, it must push forward against the teeth in order to swallow, creating what is commonly referred to as a tongue thrust.
Mouth breathing is capable of altering your face’s shape and appearance due to the positioning and functioning of the tongue, mouth, and facial muscles.
Symptoms of untreated mouth breathing can include long, narrow faces and jaws, ill-defined cheekbones, recessed chins, “gummy smiles,” and crooked or crowded teeth.
Mouth breathing can also affect the positioning of teeth. Lips typically provide external support for the teeth. However, when the mouth is perpetually open, this external support is decreased as the lips become weakened. The low-lying tongue that goes part and parcel with mouth breathing simultaneously pushes forward instead of upwards at rest and during swallowing, progressively causing the teeth to shift over time.
As you might imagine, this can cause problems with orthodontic treatment. Specifically, a longer time spent in braces is likely to be required. It is also a strong possibility that those treatment results won’t be permanent, resulting in additional orthodontic needs down the road.
Nasal breathing is linked with “diaphragmatic” or slow, deep breathing, which triggers our bodies’ rest and digest parasympathetic nervous system functioning (i.e., our relaxation response).
On the other hand, mouth breathing involves “chest breathing,” which is a more rapid and shallow breathing pattern associated with our bodies’ fight or flight sympathetic nervous system functioning (i.e., our stress response). When our bodies are chronically functioning in this fight or flight response pattern, it leads to systemic inflammation, which ultimately takes a toll on our physical, mental, and emotional health by contributing to illness and disease.
Quite basically, regularly using the mouth for breathing contributes to an imbalance of oxygen and carbon dioxide, as well as changes in hormones, blood sugar levels, etc. within our bodies. Mouth breathing thereby disrupts many aspects of our bodies’ natural functioning. Symptoms can include, but are not limited to:
- Headaches
- Dry mouth
- Bad breath
- Gingivitis and periodontal disease
- Cavities
- Sore throat
- Cold symptoms such as mucous production and blocked nasal passages
- Impaired sleep and chronic daytime fatigue
- Anxiety and depression
- ADD and ADHD symptoms
- Impaired academic performance
- Digestive disturbances such as gas or bloating, acid reflux, etc.
- Heart problems
- High blood pressure
- Poor growth and development
Mouth breathing further contributes to muscle imbalances from the neck down, leading to postural and mechanical issues throughout the body. Basically, when the mouth is open and the tongue is positioned low and forward, the head tends to also be pulled in a forward direction, affecting neck, shoulder, and back posture. Spine, ribcage, and lower body alignment is subsequently affected as the body attempts to seek balance. Structural misalignments ultimately alter the mobility and function of these body parts, contributing to compensatory mechanics during daily activities. You can imagine the ill-effects of such compensations on muscles, connective tissues, and joints over time.

Physical Therapy Interventions
“The thigh bone’s connected to the hip bone. The hip bone’s connected to the backbone…” Most of us appreciate the fact that our bones are interconnected to comprise our skeletons. However, it seems we often take for granted that the rest of our tissues are interconnected, as well.
The tongue is a muscular organ in the mouth. But how amazing is it that the tongue is actually connected via fascia to multiple other points throughout the body, all the way down to the toes? Fascia is a thin casing of connective tissue that surrounds, protects, and holds every organ, blood vessel, bone, nerve fiber, and muscle in place within our bodies. Likewise, neuromuscular connections are coordinated throughout our bodies from head to toe.
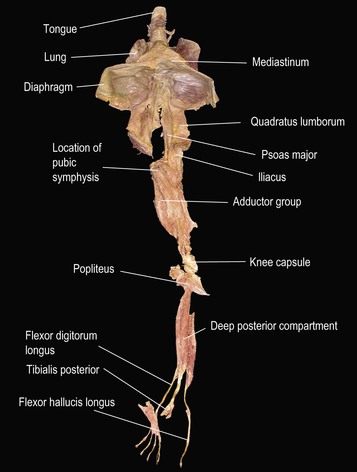
While the mouth and tongue are reasonably considered as usual suspects in TMJ and swallowing disorders, they all too often are not considered as pertinent factors in issues that appear elsewhere in the body, and vice versa. Yet orofacial myofunctional disorders frequently go hand in hand with concerns related to posture and alignment, gait and other biomechanics, pelvic floor function, and more.
Utilizing a whole-body approach to orofacial myofunctional concerns can ultimately provide more effective treatment. Our bodies, including muscles and functions from the neck up, require a stable base and balanced system from the neck down in order to work efficiently.
Through the incorporation of traditional and non-traditional physical therapy interventions with orofacial myofunctional treatment techniques, we can essentially address issues from multiple angles to optimally impact the whole body’s function.
Interdisciplinary Treatment
Although I wish it was possible, I know all too well that no one person can be an expert at everything. That’s why I rely on a team approach to patient care.
Building strong relationships with trusted colleagues within various specialties allows me to focus on what I do best, and enables me to help my patients get the thorough care they need and deserve.

I use every session with patients as an opportunity to screen for interdisciplinary provider needs. Some of the professionals I collaborate with include therapists (e.g., physical, speech, occupational, vision, massage, etc.), orthodontists, dentists, chiropractors, ENTs, allergists, dieticians and nutritionists, lactation consultants, sleep specialists, pediatricians, family physicians, functional medicine practitioners, counselors, and more.
With consent, I am happy to maintain open communication as appropriate with any practitioners involved in my patients’ care to ensure the best possible outcomes.

Oral Habit Elimination
Habits such as finger or thumb-sucking are often used as forms of self-regulation for young children, while such things as nail biting or lip sucking are common outlets of anxiety for adults.
Although they might be effective in these ways, such habits unfortunately also contribute to altered mouth and facial muscle use, malalignment of teeth, and they force the tongue to be in a low-resting position in the mouth. This ultimately adversely affects breathing and orofacial development, as well as such things as swallowing, speaking, and posture.
With proper training, it is possible to eliminate these habits, develop more effective nervous system regulation skills, and improve the development and function of mouth and facial muscles for long-term health. Oral habit elimination is an important first step of an effective overall orofacial myofunctional therapy program.
Supportive Interventions
- Nasal Release Technique (NRT)
- Also referred to as: Endonasal Technique, Cranial Facial Release, Nasal Cranial Release, Bilateral Nasal Specific Technique, Functional Cranial Release, and NeuroCranial Re-Structuring, Nasal Specific Technique
- Craniosacral Fascial Therapy (CFT)
- OraLase
- PerFacT
- At-home sleep studies
- Various lab testing options
- Food and environmental sensitivities
- Vitamin, mineral, omega levels
- Nutrigenomics
- Gut microbiome

Services We Provide

Cognitive Behavioral Health

Cosmetic Concerns

Dental/Oral Health

Digestion/Eating Issues

Ear/Nose/Throat Health

Exercise/Activity Restrictions

Musculoskeletal Issues

Oral Habit Elimination

Respiratory Health

